Human Reproduction Class 12 | Chapter 3 | Biology | CBSE |
Table of Contents
Human Reproduction Class 12 | Chapter 3 | Biology | Class 12 | CBSE |
Reproduction is the process by which an organism produces young individuals of its own species. It helps in maintaining the continuity of the species.
Sexual Reproduction
Males and females produce cells specialised for reproduction, which are called sex cells or gametes. The male sex cells are called sperm cells and female sex cells are known as ova. The fusion of sperm with an ovum produces, a zygote. The single – celled zygote have all the chromosomes present in the two gametes. A Multicellular embryo forms by the Repeated mitosis of the zygote which gradually develops into a full – grown animal.
Human reproductive Systems
Male reproductive system
The male reproductive system is located in the pelvic region. It includes a pair of testes along with accessory ducts, glands and the external genitalia.
Testis
Testis are the primary sexual organs of males. There are two testes, each testis is a small, pinkish and oval, with a length of about 4 – 5 cm and a width of 2 – 3 cm.
Testicular lobule – Testis get divided into the small compartment known as Testicular lobule and each testicular lobule contain 1 – 3 highly coiled tubular structure known as Seminiferous tubule.
In between the seminiferous tubule, interstitial space present that contain the special cell known as Leydig cell or Interstitial cells.
One end of the Seminiferous tubule is closed and other open tubular end is known as Tubuli Recti that open in the lumen of the testis.
Tubuli Recti of all seminiferous tubule get highly cross link within the lumen of the Testis and form a network known as Rete Testis.
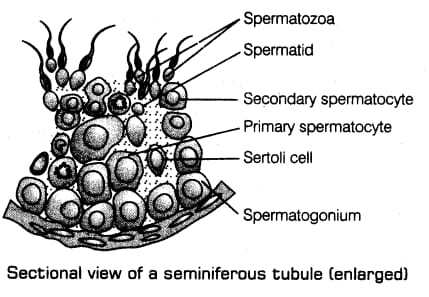
Seminiferous tubule
The outermost protective layer of the Seminiferous tubule is made up of cuboidal epithelium.
In seminiferous tubule, two type of cell present.
Spermatogonia – Small, round cell that undergo division and give rise to the sperm.
Sertoli cell – Long elongated cell that provide nourishment to the developing sperm.
- In between seminiferous tubule, leydig cell present that produce the Androgen hormone under the influence of ICSH (intra cell stimulating hormone) or LH hormone.
Scrotum
It is pink colour pigmented like structure in which testis get descend during the 7th month of embryonic development.
Testis descend through the Inguinal canal.
Internally scrotum is divided into two chamber with the help of a septum scorti.
The end of the Testis attach to the scrotum with the help of a fibrous Structure known as Gubernaculum.
Scrotum sac help in Thermoregulation i.e. maintain the proper Temperature for the Spermatogenesis.
Testis required 2 – 2.5 less Temperature than the body temperature. So, to get the proper Temperature testis get descend into the scrotum sac.
Vas Efferentia
Small duct arise from Rete testis and that carry the sperm form Rete testis to the Epididymis.
It is made up of ciliated epithelium.
- Tubuli recti, Rete testis and Vas efferentia form the intra Testicular duct system (ITDS).
Epididymis
Long, narrow, highly coiled, muscular tube like structure.
It secrete the specific factor that help in Maturation of sperm.
It is made up of Pseudostratified epithelial, and have sterio cilia, and sperm move due to the peristalsis movement.
Epididymis divided into three parts :-
→Head part known as Caput Epididymis.
→Middle part known as Corpus Epididymis.
→Tail part known as Cauda Epididymis.
Vas deferens
Vas deferens is a straight tube with a thick, muscular wall. It is made up of Pseudostratified epithelial.
It carry the sperm from the tail part of the Epididymis upto the seminal vesicle.
Ejaculatory duct
Small duct that form by the combination of vas deferentia and seminal vesicle tube.
It carry the sperm upto the urethra.
Urethra
Urethra of male serves a dual function, which involves both the reproductive system and urinary system.
Penis
It is a eractile copulatory organ that help in incersion of sperm within the female body during the sexual intercourse.
Accessory Genital Glands
Seminal vesicles
There are paired seminal vesicles which are sac – like structure It is present at the base of urinary bladder.
It contributes 60 percent in semen and it have a pH of 7.4 .
They secrete substances that are fructose which provides energy for locomotion, Citrate is nutrient for sperm.
Prostglandins the semen may stimulate contractions of the female uterus, which help in moving sperm up to the female reproductive tract.
Prostrate Gland
A single prostate gland is there which present on the surrounding of Prostatic urethra.
Have a pyramidial shape and have slightly acidic pH (6.5)
It contains Citrate, Prostglandins enzyme.
It contributes 20 – 25 percent of semen and it gives milky appearence to the semen..
Bulbourethral glands (Cowper's glands)
A pair of bulbourethral gland is present on surrounding of membranous urethra which is pea shaped.
It contributes 10 percent of semen and have alkaline pH (7.4).
It contains mucus ions (Lubricant).
Functions
- Alkaline pH neutralise the acidic pH of the urethra and female reproductive tract.
- Lubricant lubricate the urethra and female reproductive tract and minimise the sperm damage during the sexual intercourse.
Seminal fluid
It is the collective secretion of Testis, accessory duct and accessory gland that come outside the penis during the sexual intercourse.
Single ejaculation may vary from 3 – 5 ml/ejaculation.
There are usually between 200 – 300 million/ ejaculation in which 60 percent sperm that have proper shape and size and 40 percent vigrous activity.
Female Reproductive System
The female reproductive system consists of two ovaries, oviduct, uterus, cervix, a vagina and the external genitalia, accessory genital glands and the mammary glands.
Ovaries
Ovary is the primary sex organ where the female gamate and different steriod hormone get form.
There are two ovaries which are almond shape.
Location – Lower abdominal cavity and its origin is abdominal.
Ovaries divided into 4 region:-
Outermost layer is known as Germinal epithelial and inner to the germinal layer Fibrous connective tissue present known as Tunica Albugenia.
Inner to the Tunica Albugenia, Peripheral region is known as Cortex and the innermost region of the ovary in which blood supply occur in known as Medulla.
Hilum – It is the region through which blood vessel, lymphatic vessel and nerve fibre get enter.
Cortex region – Different follicular changes within the ovary takes place in cortex region in the ovary.
Fallopian tubes
It is a tubular structure that arise on the lateral side of the uterus and which is upto the ovary.
Parts of fallopian tube
- Infundibulum – Anterior funnel shape part of the fallopian tube.
At the tip 0f infundibulum, finger like projection present known as Fimbriae.
Fimbriae enclose a small pore or opening known as Ostia through which 2° oocyte get enter within the lumen of the fallopian tube.
- Ampulla – Widest and longest part of the fallopian tube.
It is the site of fertilization.
- Isthmus – Small, narrow part of the fallopian tube that open within the Uterus.
Functions of Fallopian tube
- Convey ovum to the uterus.
- Provide the site of fertilization.
Uterus
Also known as Womb. It is inverted Pear shape.
Location: It is situated above and behind the urinary bladder and remains attached to the body wall by Ligaments.
- It can extend itself upto 100 times in size to accumulate developing foetus.
Parts of the uterus
Fundus – The upper dome shaped structure .
It is the site of implantation.
Body – The middle, large and widest part of the uterus.
Cervix – The narrow, small opening part of the uterus.
It enclose a cavity that is filled with the mucus known as Cervical canal.
Structure of Uterus
Epimetrium – The outermost made up of visceral peritonium.
Myometrium – Made up of smooth muscle. It help in Parturisation.
Endometrium – The innermost glandular epithelial, it undergo cyclic change to release the unfertilized ovum outside the body.
It is the part of uterus where foetus get implanted.
Vulva
Mons Pubis – It is anterior fleshy, prominent part and have the deposition of the fat (adipose tissue).It have the pubic hair and it present over the pubic synphysis.
Labia majora – Homologous to the Male scrotum
The outermost fleshy fold that is larger in the size and have the hair on the outer side.
Labia Minora – Homologous to the penile urethra. It is small, thin fold i.e. enclose within the labia majora and do not have pubic hair.
Clitoris – On the anterior part where labia minora get fuse from a small finger like projection known as clitoris. The tip of clitoris is known as glans clitoris and it is covered by a small skinny fold known as foreskin or perpuce.
Clitoris is homologous to the male penis.
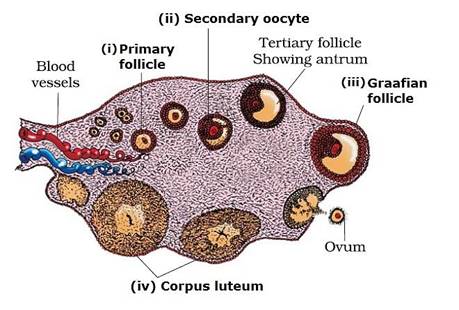
Internal Structure of Human Ovary 
- During the third month of the foetal age, germinal epithelial undergo mitotic division and give rise to oogonia or ovum premodial cell.
- In the foetal age of the development, the first phase of the oogenesis get completed and now no more premodial cell added and approximately 4 – 5 million precursor get form.
- These oogonia undergo the growth phase and get enlarge in the size and become 1° oocyte and start its meiotic division but get arrested in the diplotene phase of prophase I of meiosis.
- Follicular cell of the ovary get accumulate around the I° oocyte and give rise to the structure known as I° Follicle.
- From foetal age to the puberty large number of 1° Follicle get degenerate and the process of degeneration is known as Follicle atresia and the follicle that get degenerate is known as Atretic follicle.
- At the time of puberty, under the influence of the FSH hormone, Follicular cell undergo change in shape and become cuboidal and start division to form the multi layer structure around the oocyte and the cuboidal cell that form around the primary oocyte are known as Granulosa.
- Primary follicle get transform into 2° follicle as the multilayer structure of granulosa cell formed around the 1° oocyte.
- Granulosa cell start secreting a liquid that lead to formation of a cavity and the cavity that form is known as Antrum and granulosa cell start differentiating into two layer i.e. Theca externa and theca interna and due to all these changes 2° follicle get transform into 3° follicle.
- In the 3° follicular stage, theca interna start secreting estrogen hormone and 1° oocyte complete its Meiosis I and become 2° oocyte and due to the unequal cytokinesis a small size polar body form that undergo degeneration.
3° Follicle get enlarge in size and become mature graffian follicle.
- In the mature graffian follicle, 2° oocyte form a protective layer around itself by secreting specific chemical that is protective in nature and known as Zona pellucida and outside the zona pellucida, ovary cell form other cellular structure that is known as Corona radiata.
- The peak level of LH hormone get reach and it is known as LH surge and it cause ovulation i.e. release of 2° oocyte from the mature graffian follicle in the oviduct.
- LH hormone start deposition of luteal pigment within the remainings of the graffian follicle and the structure that form is known as Corpus luteum and it is of yellow colour which is the source of progestrone hormone.
- Progestrone hormone inhibit the GnRH that stop the secretion of LH hormone from the pituitary gland and due to the decrease in LH hormone, corpus luteum start degenerating and white colour degenerating corpus luteum is known as Corpus Albicans.
Mammary Gland in Human Female
Mammary glands are modified sweat gland and present in both the sex. But in the female it get enlarge under the influence of the estrogen and progestrone hormone.
It develop on the pectoralis major chest muscle. The tip of the mammary gland containing prominent round structure known as nipple. In the surrounding of the nipple, Melanin get secreted and form the pinkish region and that have areolar gland.
Mammary glands contain 15 – 20 lobular structure known as Mammary lobule that contain the small alveoli. The epithelial of the alveoli secrete milk and a small duct arise from the alveoli known as Mammary tubule.
Mammary tubule open into a large duct known as Mammary duct. Mammary duct get swollen and form a sinus known as Lactiferous sinus, where for the temporary time period milk get store.
A small duct arise from lactiferous sinus that get open into the nipple.
Events of Human Reproduction
The process of the formation of gamates is called Gametogenesis. There are two types of gamates, the spermatozoa and ova.
Spermatogenesis
Spermatogenesis is the process of the formation of male gamate i.e. sperm. It takes place in seminiferous tubules of the testes.
Spermatogenesis is completed in three major steps:
(1) Spermatocytogenesis. In this process, spermatogonia divide and produce successive generations of cells that give rise to spermatocytes.
(2) Meiosis. In this phase, the spermatocytes go through one reduction division (meiosis I) and one equational division (meiosis II).
(3) Spermiogenesis. It involves no cell division . In this process, the spermatids differentiate into spermatozoa.
Human Sperm
The mature Human sperm have three parts :
- a head
- a middle piece
- and a tail
The head of a sperm contains the nucleus having a haploid set of chromosomes in a compact and inactive state. It is covered by a specialized Acrosome.
Acrosome contains Hydrolytic enzymes needed to penetrate the egg.
The head is followed by the cylinderical midpiece, which contains the mitochondria which provide energy. There are two distinct granules – the proximal and distal centrioles. The proximal centrioles plays a crucial role during the first division of the fertilised ovum. The distal centriole gives attachment to the axial filament of the long tail of the sperm. The sperm locomotes by the undulating movement of the tail.
Hormone Regulation 
Functions Of Sertoli cells :
- It provide nutrition to the developing sperm.
- It secret the specific factor that help in conversion of spermatid into spermatozoa.
- It secret ABP that help in increasing the concentration of Testosterone within the seminiferous tubule that initiate the process of Spermatogenesis.
- It secret inhibin that regulate the process of Spermatogenesis.
Oogenesis
Oogenesis is the process of formation of female gamate i.e. ovum.
Menstrual Cycle
The cyclic changes in the reproductive tract of the human female extend over 28 days, but variations form 24 – 35 days are normal, and greater variations are not uncommon.
- The menstrual phase in which the endometrium is shed from the body.
- The proliferative phase in which the regeneration of endometrium takes place.
- The secretory phase in which the nutrients are secreted by endometrium for implantation.
Menstrual phase
The menstrual period occurs on days 1 to 5 of a new cycle. There is some individual, however. During this period, considerable parts to the mucous membrane and glands are broken down and lost from the linings of uterus, Fallopian tubes and vagina. This thins out their mucosae. The blood vessels of the uterine are also ruptured to cause the bleeding.
Proliferative phase
On second day of the cycle, follicle stimulating hormone (FSH) releases by the pituitary gland. The stimulates the developments of several ovarian follicles follicles. At around 6th day, one of the follicles dominates and starts to secrete estrogen. The other degenerate. The remaining follicle develops into a Graafian follicle and continues to secrete estrogen until dyad 14 of the cycle. Consequently, blood estrogen levels rise. Estrogen hormone causes proliferation (growth) of the endometrium to remake the layer lost during the previous menstruation. The repair is complete after 14 days.
Secretory phase
Luteinising hormone has a second effects; it causes the Graafian follicle to develop into a corpus luteum (yellow body). The yellow appearance of the secetory cells that develop inside the ‘remains’ of the Graafian follicle. The corpus luteum secrets estrogen and progesterone. Progesterone cause spiral – shaped blood vessels to grown into the endometrium. This thickened lining begins to secrete nutrients and mucus to prepare for and embryo to be implanted.
During this phase, production of FSH is inhibited by the high levels of progesterone. As long as level of progestrone is high, the endometrium remains maintained and new follicles are not stimulated.
If the egg cell is not fertilized, the corpus luteum lasts for about 10 to 12 days and then degenerates, cesing secrete progesterone. The is a key event because the inhibition of FSH is lifted. The endometrium is no longer protected and the cycle can star again.
Menopause
The permanent stoppage of the mestrual cycle and the cessation of ovarian activity is known as Menopause. The onset is at about the age of 50, but varies greatly. Menopause is usually uneventful, but some women suffer form complications such as flushing, excessive bleeding, and nervous disorders.
Ova are often classified according to the amount and distribution of yolk. The amount of yolk influences the pathways of development but not the final outcome. Yolk with large amount interfere with cleavage and migration.
Ovulation
Ovation is the rupture of the mature follicle with expulsion of its ovum into the pelvic cavity occurs frequently on cycle day 14 in 28 – day cycle. On day 12 to 13, the blood estrogen level reaches as threshold level, which triggers the release of lutenising gland. The speedy increase in LH levels triggers ovulation around day 14 as the ovum lives for only 24 to 36 hours.
Structure of Human Ovary 
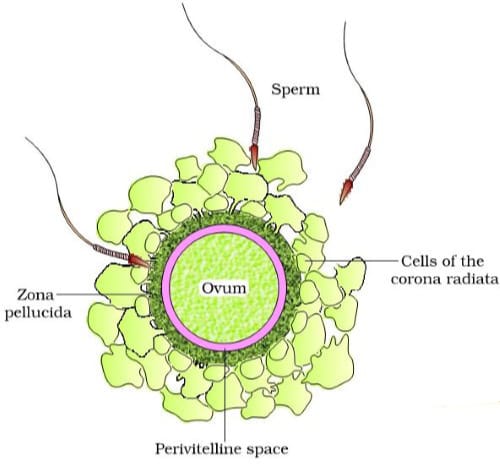
The human ovum is a rounded, non – motile cell. It is almost yolk free and it is alecithal. It has abundant cytoplasm and a nucleus present in centre. The ovum is surrounded by vitelline membrane.
Two additional egg coats enclose the ovum: inner thin transparent, noncellular zone pellucida and outer radiate. The cells of corona radiata. The corona radiata is formed of follicular cells. The cells of corona radiata continue to grasp to the ovum for sometime after the ovum is released.
Fertilization
- Arrival of Male gamate :- After the insemination of the sperm within the female body, sperm get coagulate within the female body.
Profibrilysin get activated after the 15 – 20 minutes of insemination and release of the sperm from the coagulate.
Sperm use Fructose as a energy source and move and travel with 1.5 – 3 mm/minute speed and reaches the fertilization site.
Sperm take 5 – 6 hour to reach at fertilization site.
- Capacitance of Sperm :- When the sperm passes through the female tract, inhibitory particle and cholestrol that present in the membrane of the acrosome get remove and the capacity of the sperm to get the fertilise is increase.
- Arrival of Female gamate :- After the ovulation, female gamate arrive at ampulla – isthmus junction.
- Acrosome Reaction :- Sperm come in contact of the female gamate and release different type of hydrolytic enzymes, that help in the penetration of sperm within the female gamate.
The enzyme hyaluronidase helps in degrading the Hyaluronic acid and corona radiata cell get dispersed.
Corona radiata penetrating enzyme – It help the sperm to penetrate through the corona radiata, by causing lysin of corona radiata cell.
Zona lysin – Sperm membrane get fuse with zona pellucida as zona lysin cause lysis of zona pellucida.
- Prevention of Polyspermy :- It occur in two step.
Fast block – As sperm come in contact with ovum, ovum get depolarize and other sperm is not able to penetrate the female gamate.
Slow block/ Cortical reaction – Cortical granule that present under the egg membrane get diffuse from the egg membrane into the peri vitelline space and harden the zona pellucida and remove all the receptor present on the zona pellucida.
- Completion of Meiosis II :- Sperm provide APC(Anaphase promoting complex) that help in completion of Meiosis II of female gamate and release of 2° polar body.
- Amphimixis :- Pro nucleus of male and female gamate get mix and lead to the formation of diploid nucleus.
Embryonic Development
The embryogenesis phase consisting of rapid cell divisions following by fertilization is called cleavage. The mitotic divisions during this phase are called cleavage divisions. Resulting daughter cells are known as blastomeres.
Cleavage is distinctive embryological process, which transforms the single fertilised egg cell into a sphere of closely aggregated multitude of cells. Immediately after fertilisation the zygote undergoes a series of cell series of cell divisions. The zygote divides repeatedly in close succession. The divisions are called cleavage divisions. The zygote firstly divides to form a two – celled embryo. Then each of these cells undergo mitotic division bringing the number of cells to four. Number of cells increases by repeated divisions, called blastomeres, that makes the embryo. 16 – celled, solid mass that look like mulberry is known as Morula.
The cells of morula get differentiated into the
(i) The peripheral cells and
(ii) the inner cell mass
The peripheral cell known as trophoblast, which are sticky and phagocytic in nature and help in implantation.
The inner cell mass are stem cell and give rise to the complete embryo. The trophoblast cells secrete fluid into the morula to form the blastocyst.
The early embryo get attached to the lining of the uterus is called implantation. It occurs at the blastocyst stage of development, six to eight day after ovulation.
After implantation,the endometrium undergoes changes and it called the decidia. The deciduas tissues can be distinguished into deciduas basalis, situated between the embryo and uterine serosa (mymometrium); deciduas capsularis, between the embryo and the lumen of the uterus, and deciduas parietalis, the remaining part of deciduas.
The process, by which the blastula becomes as three layered embryo, or gastrula, is called gstrulation. The blastocyst (blastula) undergoes gstrulation to produce the three primary germinal layers. This involves movements of cells that eventually help to attain new shape and embryo morphology. These cell movements are called morphogenetic movements. These movements result in the formation of there primary germinal layers, namely ectoderm, endoderm and mesoderm. During this, the blastocoel cavity of blastula is replaced by new cavity – archenteron, the primitive gut. Each primary germinal layer destines to develop specific organs and organ systems is an individual.
Following are the tissues, organs and organ systems are formed form the three layers.
(i)Ectoderm : It differentiates into structures like skin, glands of skin (sweat, sebaceous, and mammary glands), brain, spinal cord, nerves, lens of eye and inner ear.
(ii) Mesoderm : It differentiates into varieties of other structures like notochord, muscles, heart, blood vessels, kidneys, gonads, etc.
(iii) Endoderm : It differentiates into the primitive gut. The primitive gut (also called archenteron), in turn, forms the different structures of digestive and respiratory system, the urinary bladder – the middle part of he ear.
Extraembryonic of Foetal membranes
The members situated outside the embryo proper are called extraembryonic or foetal membranes. The membranes are amnion, chorion, allantois and yolk sac.
Amnion is the innermost of the embryonic membranes. It forms a fluid – filled sac (the amniotic sac) round the embryo. It prevents desiccation of the embryo. It prevents desiccation of the embryo and function as shock absorber.
Chorion is the outermost of the embryonic membranes. It completely surrounds the embryo. It protects the embryo and forms placenta for metabolic exchange between the foetus and the mother.
Allantois is the innermost of the embryonic membranes. Around the embryo, a fluid – filled sac (the amniotic sac) is formed by allantois. It prevents desiccation of the embryo and function as shock absorber.
Yolk sac is formed below the embryo. In human, egg is devoid of yolk, it provides no food for the embryo. It is very small and gradually degenerates and shrinks. It is non functional in human beings. It is the equivalent of much larger, functional yolk sаc of reptiles and birds.
Placenta
It is a interdigitation between the chronic villi and uterine tissue.
Composed of maternal and embryonic tissue, it links the blood supply of the embryo to the blood supply of the mother, allowing the exchange of oxygen, nutrients and waste products. The two blood system are not in direct contact, but are separated by thin membranes, with materials diffusing across form one system to the other.
Functions of Placenta
It serves as barrier between the foetus and the mother. It acts as an ultrafilter; soluble inorganic and organic materials nutrients, hormones, antibodies against diphtheria, small pox, scarlet fever, measles, etc. can pass form the mother to the foetus.
It helps in the gaseous exchange between the mother and the foetus. The placenta also helps in the elimination of nitrogenous discharge and other wastes of the foetus.
It acts as an endocrine gland and synthesis large quantities of proteins and some hormones, such as human chorionic gonadotropin (hCH), chorionic thyrotropin, chorionic corticotrophin, chorionic, somatomammotropin (hCG), estrogens and progesterone. The hCG signals the corpus pregnancy has begin. In response, the corpus luteum increases in size and release large amounts of progesterone and estrogen. These hormones stimulate continued development of the placenta and the endometrium.
It secretes relaxin that helps parturition by softening the connective tissue of the symphysis pubica.
During the first trimester (first months) of pregnancy, the essential structure of the body is formed. This involves division of cell, cell migration, and the differentiation of cells into the many types found in the baby. Gastrulation occurs during the second and third weeks of development. The notochord begins to from and induces formation of neural plate. The neural tube develops, and the forebrain, midbrain, and hindbrain are develop by the fifth week of development. A week or so later the for brain begins to grow outward, forming the rudiments of the cerebral hemispheres.
During this period, the developing baby called foetus. By 3 months, all the system of the baby have been formed, at least in a rudimentary way. Development of muscle is there, and the embryo becomes capable of movement. Although small, it has a recognisable human appearance. From then on, development of the foetus is mainly a matter of growth and minor structural modifications.
Parturition and Lactation
Gastration period – The time period after the concieve upto the full term expulsion of fully develop foetus or baby.
In humans, gastration period is of nine months.
The process of giving birth is called parturition. Powerful contractions of the uterus in labor are needed for parturition. The anterior pituitary of mother begins to secrete oxytocin and the placenta secretes prostaglandins, two hormones that actively promote contractions. Oxtocin stimulates uterine contractions at about 40 weeks.
There are three stages of labour
- The dilation (opens) of cervix.
- The foetus is pushed out of the uterus.
- The placenta and umbilical cord are expelled.
Colostrums
Colostrum is the first milk the breasts produce in the early days of breastfeeding. This special milk is low in fat, and high in carbohydrates, protein, and antibodies to helps keep your baby healthy. It is extremely easy to digest, and is therefore first food for your baby. It is low in volume but high in concentrated nutrition for the newborn Colostrum has a laxative effect on the baby, helping him pass his early stools, which aid in the excretion of excess bilirubin and helps prevent jaundice. After three or four days of delivery, the breasts begin to secrete milk. Synthesis of milk is stimulated by the pituitary hormone prolactin (PRL). Its release is stimulated by a rise in the level of oxytocin when the baby begins nursing. Milk contains an inhibitory peptide that inhibit the secretion of prolactin hormone.
# Human Reproduction Class 12
# Human Reproduction Class 12 Notes
# Human Reproduction Class 12 NCERT Solutions
# Human Reproduction Class 12 Biology
Do share the post if you liked the notes of Human Reproduction Class 12, Biology. For more updates, keep logging on BrainyLads.